The stakes to optimize core clinical revenue and cash have never been higher for academic providers. Although providers as a whole experienced an uptick in performance in 2024, celebration across the industry has been subdued throughout Q1 of 2025, as several headwinds continue to brew that are expected to hinder bottom-line performance.
While inflation has stabilized over the first three months under the new administration and providers have experienced 5%-6% top-line growth, reimbursement headaches continue.
These include:
- Continued payer mix deterioration
- Increased payer friction
- Reimbursement rates for commercial, Medicare and Medicaid that lag expected expense growth
- Increased competition within the hospital sector and across the care continuum
Exacerbating the top-line challenges are continued increases in expenses (7%-10%+), as well as ongoing workforce challenges attributed to increased patient acuity and complexity.
Academic medical centers face unique challenges
Academic medical centers (AMCs) are the backbone of medical innovation and training in the United States, with a three-part mission:
- Delivering cutting-edge care
- Educating the next generation of healthcare professionals
- Conducting groundbreaking research
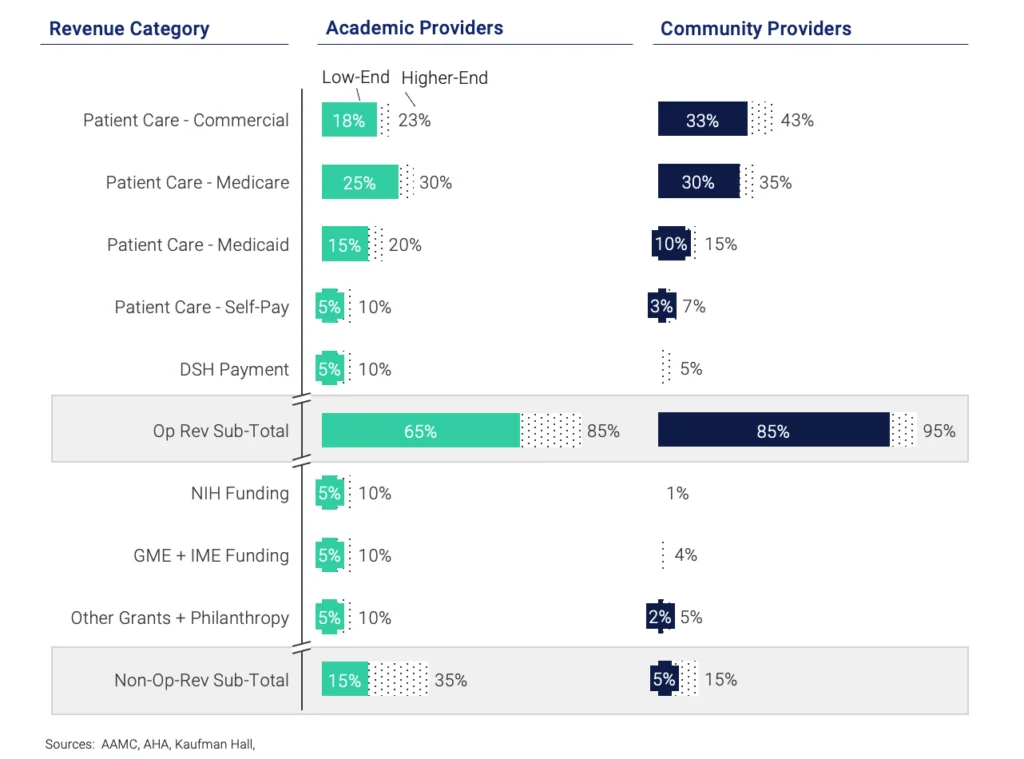
Compared to their community provider counterparts, AMCs face an even greater and unprecedented challenge: balancing their tripartite mission while grappling with escalating costs and shrinking revenue streams for both operating and non-operating revenue, whereby non-operating revenue can account for up to 35% of total revenues.
2025 is a critical juncture and inflection point for AMCs as they face continued financial suppression. This makes patient care collections not just a revenue source, but a lifeline for sustaining their unique role in the healthcare ecosystem.
The tripartite mission is under threat
According to a 2023 report from the Association of American Medical Colleges (AAMC), AMCs account for just 5% of U.S. hospitals but provide 37% of all charity care, 26% of Medicaid hospitalizations and a disproportionate share of complex cases.
AMCs’ three-part mission of patient care, education and research is expensive, and the commitment comes at a cost. It’s one that is increasingly difficult to bear as traditional revenue streams like government funding, grants and reimbursements face compression. This is demonstrated by operating margin erosion from 2017 to 2023, and anticipated declines into the foreseeable future.
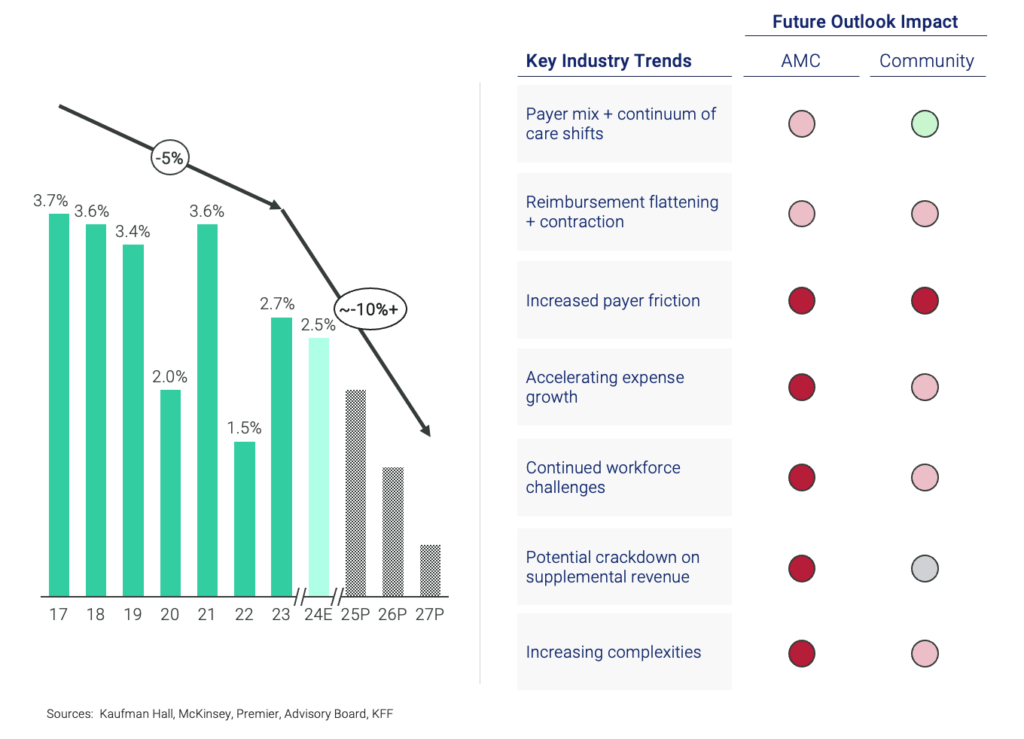
Historically, AMCs have leaned on a mix of clinical revenue, research grants and philanthropy to fund their operations, but these sources are under siege due to changing legislation, shrinking traditional patient care and non-traditional reimbursement sources, rising costs, continuing payer friction and other industry trends. These pressures include:
- Payer mix and continuum of care shifts: Despite modest revenue growth, AMCs will feel the squeeze of caring for heavy MCR/MCD/uninsured patients, increases in uncompensated care, and a continued shift to lower cost of care settings.
- Reimbursement flattening and contraction: All providers continue to face possible cuts to MCR physician fee schedule, and MCR IPPS and Medicaid rate hikes that lag expense growth.
- Increased payer friction: Increased initial and final denials (21% CAGR from 22-24 and growing), plus increased cost to collect while seeing declines in cash collections / NPR.
- Accelerating expense growth: The cost to treat, educate, research and innovate is much higher given the patient profile and mission components that go beyond a traditional hospital, and is without immunity from tariff legislation.
- Continued workforce challenges: Due to the higher complexity and acuity of AMC patients, the labor needs are typically more specialized and heightened given the need to care for sicker patients, and training and educating providers.
- Potential crackdown on supplemental revenue: AMCs are often reliant on patient care dollars and other streams to fund their entire mission; they are also grappling with potential 50% cuts to NIH funding and potential slashes to IME, GME, DSH and other programs.
- Increasing complexities: As the population ages, workforce challenges intensify and potential funding streams dry up, the ability to deliver quality patient care while training the next generation of providers will get more difficult.
While certain movements in DC and evolving payer mix dynamics are less controllable, placing an emphasis on collecting patient care dollars is more controllable, and has never been more important in the outlook and long-term sustainability for academic providers.
Partnership serves as a path forward
Uncollected patient balances can account for 6%-8% of total revenue leakage. For a mid-sized AMC, this could mean losing $60-$80 million annually , revenue that could otherwise fund research staff, facility upgrades or scholarships. With high-deductible health plans on the rise, patients are responsible for more costs, but AMCs often lack efficient billing systems, leading to delays and uncollected balances.
AMCs need to prioritize patient care collections by investing in advanced billing technologies and training staff to educate patients about their financial responsibilities. This can significantly increase revenue, help bend the cost curve and allow providers to not only execute on their clinical mission but also support and fund efforts for continued education, research and innovation.
The cost and ability to bend these cost and revenue pressures are difficult, however. While some providers are equipped to navigate difficulties themselves, most of the industry needs a partner to help right the ship in capturing the patient care dollars to enable and cultivate investment back into patients, providers and community as a whole.
Ensemble has a proven track record of being the partner to drive unmatched results for providers with exceptional service, underpinned by cutting-edge technology and innovation. We focus on:
- Immediate cost reduction and future risk mitigation through geographic arbitrage and scalability
- Seamless and thoughtful transition of a non-core business function to a partner that is best positioned to combat industry disruption
- Ability to reallocate financial resources to clinical care and strategic initiatives which benefit your patient population.
Clients see a 5.2% net revenue lift on average and meet 100% of year-one goals. Learn more about the Ensemble end-to-end approach >>>
The bottom line
Academic providers are facing unique pressures given threats not only to traditional revenue streams, but also to the supplemental sources of income that enable successful execution of their tripartite mission.
Most academic providers, however, are incapable of bending these pressures themselves. The right end-to-end revenue cycle management partner can help support by leading with an innovative, AI-forward approach and exceptional service, leading to unmatched results that can help AMCs stay solvent under intense headwinds.




